This Year, Carbs Are Cool!
January 10, 2019
Make 2019 A Year of Happiness
January 21, 2019Breastfeeding has been the way to nurture babies since the dawn of human history. In fact, your body will start making colostrum during the second trimester of pregnancy. Upon delivery of the placenta, progesterone is released and prolactin is stimulated to produce milk, a process known as lactogenesis. In some cases of C-sections or when placenta fragments remain in the uterus, lactogenesis can be delayed, causing issues with milk production and breastfeeding. Uncomplicated deliveries usually result in the body producing enough milk for your baby’s needs. Breastfeeding results in lower risk of obesity in baby and better postpartum recovery for Mom. Non-breast-fed babies have more risk of disease due to increased obesity. The longer a baby breastfeeds, the less chance of them becoming obese.
A healthy and realistic goal is to breastfeed for at least 6 months and continue breastfeeding in conjunction with complementary foods for one year. Foods rich in iron and zinc should be introduced at about 6 months of age. My favorite ways to sneak iron in is by sprinkling ground cumin on everything or serving meat, lentils and refried beans.
Besides water, lactose, fat and protein, human milk has hundreds of other species- specific bio active components that helps to form a unique and healthy microbiome in the gut which can prevent allergies, disease, and cancer. Babies are born with porous guts and breast milk helps to coat the lining of the stomach to prevent foreign materials and harmful bacteria from getting in the blood stream. The baby also has access to the mother’s immune system. B fighter cells from the baby’s mouth go into the mother’s breast where antibodies are made. The process of breastfeeding has effects beyond the components of milk and both mothers’ and babies’ immune systems are stronger from breastfeeding. When baby sucks on the breast, it causes the baby’s parasympathetic nervous system to trigger the release of the GI hormones gastrin and CCK (cholecystokinin) leading to increased digestion and making baby sleepy and full while decreasing the hormone, somatostatin which inhibits GI secretion, motility and the secretion of human growth hormone. This process also stimulates Mom’s digestion and improves elimination. This is one of the reasons breastfeeding helps Mom lose the baby weight so quickly as well as the fact that breastfeeding burns an extra 500 calories per day.
I am a huge believer that your thoughts dictate your life. If you think that breastfeeding is going to be too hard and super painful, then most likely it will be. It’s important to go into breastfeeding with confidence and understand that breastfeeding has been done for thousands of years and is a very natural part of the postpartum experience. Also, trust that your body and your baby will both be able to breastfeed like a boss! However, it is important to be realistic about what breastfeeding entails. It’s going to be a lot of trial and error and feeding around the clock which can be exhausting. Also, don’t let people’s limiting beliefs put doubt in your mind about breastfeeding. One of the biggest reason’s women don’t breastfeed is because of their peer’s horror stories or because they think they aren’t making enough milk for their baby. The first 3 to 7 days postpartum posed the greatest risk for stopping breastfeeding which is why it’s so important to stick with it.
Even though the United States has all the resources in the world to make breastfeeding successful such as baby friendly hospitals, lactation consultants, documentaries, books, guides, etc we have the lowest rates of breastfeeding initiation and duration compared to many other countries. Cuba, Svetlanka and Bangladesh have the highest rates of breastfeeding initiation and duration despite their limited resources.
Many times you hear that breastfeeding shouldn’t hurt and if it does, it means your not doing it right. Regardless of whether you have a perfect latch or not, breastfeeding will feel uncomfortable for the first few days or even first couple of weeks. Your nipples have never had this kind of action and stimulation before and it takes time for them to get used to a baby latching on to them 8-12 times per day. Your nipples may feel a bit raw and if so, ice packs, and coconut oil can provide some relief. It’s important to understand that while nipple tenderness is normal, cracking and bleeding is not. Your nipples will soon get tougher and breastfeeding will continue to get easier. What’s important is that you stick with it.
10 Tips for Breastfeeding Like A Boss
1. Establish Your Plan to Exclusively Breastfeed
Before getting into the how-to’s of breastfeeding, it’s important to first establish your plan to exclusively breastfeed. Exclusive breastfeeding means that the baby only get milk from the breast. Communicate this with your health care providers, spouse, family, friends, and support team. Make sure the healthcare providers in the hospital know that you do not want to formula feed for any reason unless medically necessary. A few drops of colostrum is all a newborn needs in the initial hours of birth.
Colostrum is the first milk secretion made from the breasts that are rich in antibodies and nutrition. Colostrum is much thicker and yellower in color than the breast milk that comes in a few days after birth. The thick consistency of this colostrum helps the baby learn how to swallow and feed slowly compared to a thinner milk that may flow to fast through the baby’s airways and cause choking. Not only are you learning how to feed your newborn, but your baby is also learning how to breathe, suck and swallow. This thick liquid is designed to seal the baby’s porous gut, preventing foreign substances from penetrating the digestion system and leaking into the blood stream which can cause auto-immune related disorders later on. Colostrum also acts as a laxative to help push all of that meconium out and preventing jaundice.
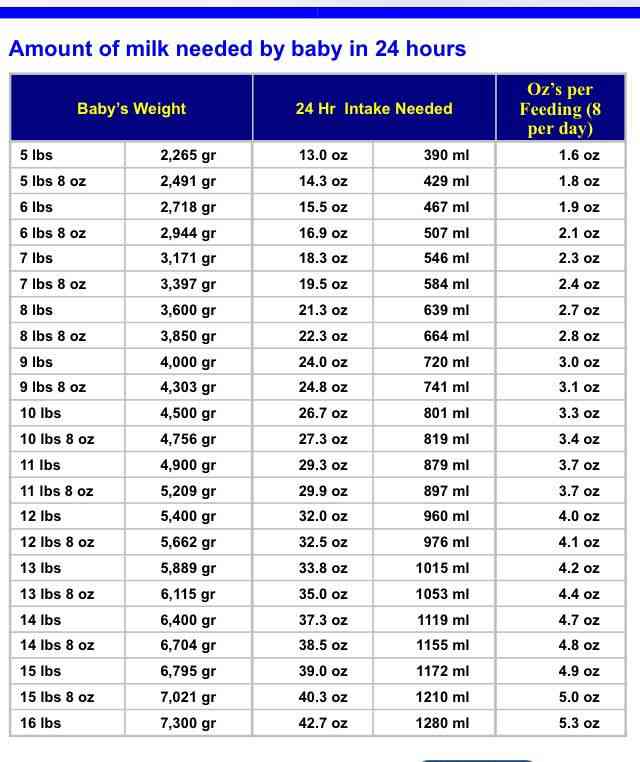
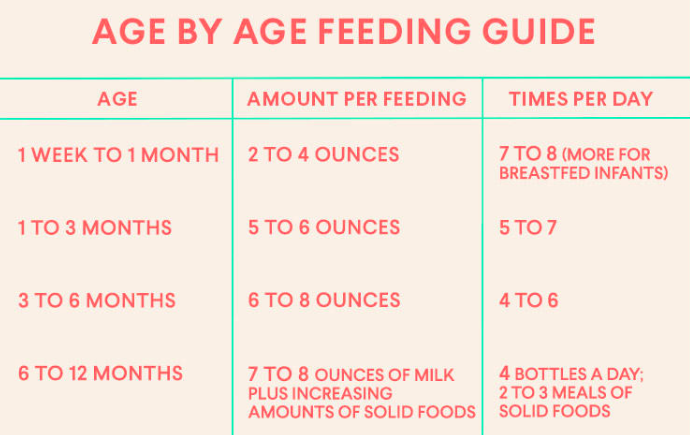
Keep in mind that a newborn baby needs very little milk in the first couple days considering that a baby’s stomach is only the size of an almond on day one. Baby’s stomach grows from the size of an almond on day one to a pin pong ball on day three, to a medium chicken egg on day seven. The amount of breastmilk your baby can hold will increase from one teaspoon (on day one) to up to two ounces (on day seven). A simple feeding calculation for the first two months is to take the baby’s weight, multiply is by 2.5 and divide it by the number of times baby eats per day to get ounces per feeding. Typically after two months, breastfed babies need between 19-30 ounces per day and take in between 3-6 ounces at each feeding.
- Newborn Intake: 78 ml/2½ ounces per feeding
- 30 ml= 1 ounce (~1 ounce per breast)
While the below information and charts are a great guide for how much to feed, trust that your baby will let you know whether they are hungry or full based on feeding cues. Ultimately, you should feed your baby on demand every 2-3 hours to keep them happy and satisfied while keeping your milk supply up. Sometimes babies will want to cluster feed, also called bunch feedings. This is a series of quick feedings given every 1-2 hours at certain times of the day. The exact reasons for cluster feeding are unknown. However, experts assume cluster feeding is a way babies boost breastmilk production.our baby’s stomach grows rapidly during the first few months of life, and your body must produce more milk to meet the increased demand. Cluster feeding may be natures way of kick-starting this process. Some mothers notice cluster feeding returns with older babies who are approaching a growth spurt or developmental leap.
How Much Baby Should Be Taking In Per Feeding
Day 1: 1 teaspoon colostrum
Day 2: 1 ounce of breastmilk (2 tablespoons)
Day 7: 1 ½ ounces of breastmilk
Day 10: 2 ounces of breastmilk
Day 14: 2 ½ to 3 ounces of breastmilk
To establish successful breastfeeding, it’s important to follow the 9 Instinctive Stages during the first hour of birth.
The Magical Hour: The 9 Instinctive Stages After Birth
Stage 1: The Birth Cry
The distinctive cry occurs immediately after birth as the baby’s lungs expand.
Stage 2: Relaxation
This stage usually begins when the birth cry has stopped, and the baby is placed skin to skin with the mother ideally, on the abdomen. The newborns hands are relaxed and there are no signs of mouth movements.
Stage 3: Awakening
The newborn exhibits small thrusts of movement in the head and shoulders and typically begins about 3 minutes after birth. Baby is feeling the sensation of no longer being confined and is finally able to stretch out and get familiar with the world.
Stage 4: Activity
The newborn begins to make increased mouthing and sucking movements as he/she starts to explore the environment with their mouth. This stage usually begins about 8 minutes after birth. The baby has more stable eye movements and looks at the breast. The dark areola around the nipple attracts the baby to the nipple area and baby will start to move their hand to their mouth, stick out their tongue and massage the breast with one or both hands. All of these movements increase the release of oxytocin in the mother which provides a sense of peace for the mother and allows her to let down her first milk supply.
Stage 5: Rest
The baby may have periods of rest between the activity stage and before the baby actually goes to the breast. This resting time does not mean the baby is disinterested in breastfeeding but rather needs time to navigate on its own on its own time.
Stage 6: Crawling
Baby “crawls” using sliding, pushing, leaping and crawling movements to reach the breast and nipple. These are short periods of action around 35 minutes after birth. The babies movements also helps the uterus contract back to size.
Stage 7: Familiarization
Baby becomes acquainted with the mother by licking the nipple and touching and massaging her breast. Baby may also make subtle sounds to get Moms attention. This stage usually begins around 45 minutes after birth and could last for 20 minutes or longer. Breast massage by the baby is the number one way to produce oxytocin in the mother. Oxytocin is the hormone that stimulates milk let down. Most likely the mother will start to leak colostrum from the nipple which the baby will smell. The properties in colostrum are similar to amniotic fluid which the baby will recognize as sustenance. Don’t try to latch the baby. The baby will do this on its own once their tongue drops to the bottom of their mouth. From there the baby should open their mouth wide (over 140 degrees) for a deep and effective latch.
Stage 8: Suckling
This is the stage where the newborn takes the nipple, self-attaches and starts to suckle. You should hear a rhythmic suck, suck swallow sound. This usually begins about an hour or so after birth. If the mother has had analgesia or an epidural during labor, it may take a while longer for baby to complete these stages as the baby is a bit lethargic and tongue may not yet work properly. With an epidural, this magical hour could be close to two hours before breastfeeding is established. Also, keep in mind that the first milk (colostrum) is very thick and concentrated to allow baby to learn the basic feeding skills and it may require stronger suckling. Colostrum is extremely nutrition and is high in protein, fat soluble vitamins, minerals, and antibodies needed for a healthy gut and immune system. Baby does not need a lot of this to keep them sustained which is why it is not needed to supplement with formula during the initial hours after birth. After 3 to 4 days, a mother’s milk supply will start to increase and will be thinner and easier for baby to feed and take in more volume.
Stage 9 – Sleep
The baby and mother fall into a restful sleep. This usually happens about 1½ to 2 hours after birth.
Milk production is positively associated with suckling in the first 2 hours after birth. Keep in mind that if you are induced/augmented, have an epidural, are given pain medication or IV fluids, it may take longer to establish breastfeeding because of a delayed onset of milk coming on or baby being lethargic from fentanyl. Fentanyl from the epidural can prevent the baby’s tongue from dropping from the roof of the mouth. Baby’s tongue must be relaxed at the bottom of the mouth to suckle correctly and create a vacuum seal for ideal milk transfer. Make sure the baby rooms in with you in the hospital to help you identify baby’s feeding cues.
Also, to establish healthy breastfeeding, it’s recommended to avoid using a pacifier since this can cause nipple confusion. A dry suck on a pacifier can also flatten the baby’s ear tube where bacteria can get caught and lead to ear aches or infections. Try to establish milk supply for 3-4 weeks before offering a pacifier. Also, try to establish your milk supply before introducing a bottle as this can also cause nipple confusion and force your baby to feed too fast. In my situation I actually introduced one bottle of breastmilk after the first week to give me time to rest in the middle of the night. By this time, my milk supply was well established since I was feeding every 2-3 hours around the clock. This once a day bottle is also a great way for my husband to bond with our son in the initial weeks. Introducing a bottle feed can also acclimate your newborn to daycare life once Mom goes back to work. If you are breastfeeding, it’s important to have someone besides yourself offer the bottle to avoid nipple confusion.
If breastfeeding is difficult for you, consult a certified lactation consultant early on. You can also find a current list of baby friendly hospitals who promote breastfeeding at www.babyfriendlyusa.org
In Chicago, I recommend JOC Lactation Consultants. They changed my life and helped my baby and I breastfeed like badasses!
2. Understand the Basics of Milk Supply & Demand
Prolactin is the hormone that makes milk. The number one way to stimulate prolactin is from nipple stimulation. Hence, the more you breast feed your baby, the more milk you will make. The less you breast feed, the less milk you will make. When the baby feeds, the nipple is constantly stimulated, and the body produces prolactin. Although it may sound exhausting, it’s important to establish a healthy milk supply by feeding your baby on demand every 2-3 hours or according to the baby’s feeding cues for at least the first 4-6 weeks post-partum. You should aim for 8-12 feedings per day for the first few weeks making sure to start immediately after delivery. 8 feeds per day, every 3 hours is ideal. You may notice baby wants to feed more frequently before bed to allow a longer stretch in the night.
Oxytocin is the hormone that moves milk also known as milk ejection reflex. The number one way to move milk is with baby hand massage on the breast and nipple stretching in baby’s mouth from a strong latch. This is why a swaddle that locks baby’s arms in place, is not the best way to feed. Baby should have arms free to allow touching of the breast. Touch stimulates oxytocin and also allows baby to have more control over its own positioning during feeding. Baby separation during initial hour or two post-partum can actually delay milk let down which is why it’s important to delay having visitors hold the baby until at least 2 hours post-delivery. Oxytocin is also the hormone that helps the uterus contract back to size and can help Mom speed up recovery and reduce blood loss.
Think about supply and demand in relation to how an ice making machine works. When ice is empty, machine makes milk automatically. The breast regulates itself in a similar way and prolactin and oxytocin go together.
Usually your body will make just the right amount for your baby. However, some women have an oversupply of milk or a fast flow. This can be exhausting for baby to take in and may lead to choking, gas and upset stomach. Baby may never be able to empty the breasts and get a satisfied feed which leaves them content. If this is the case try feeding from only one breast per feeding, making sure to burp the baby multiple times during a feed. On the next feeding, feed from that same breast again (which will contain a thicker milk that is easier for baby to swallow. Repeat this method at the next feeding on the other breast so you are feeding twice on one breast and twice on the other. This can also help to regulate your milk supply. If you find that your breast that isn’t being fed from becomes engorged, you can manually express some milk for relief. You can also try cluster feeding multiple times before bed to empty breasts and keep baby satisfied throughout the night.
Peppermint tea can also help to balance out your oversupply and can provide a soothing affect for baby.
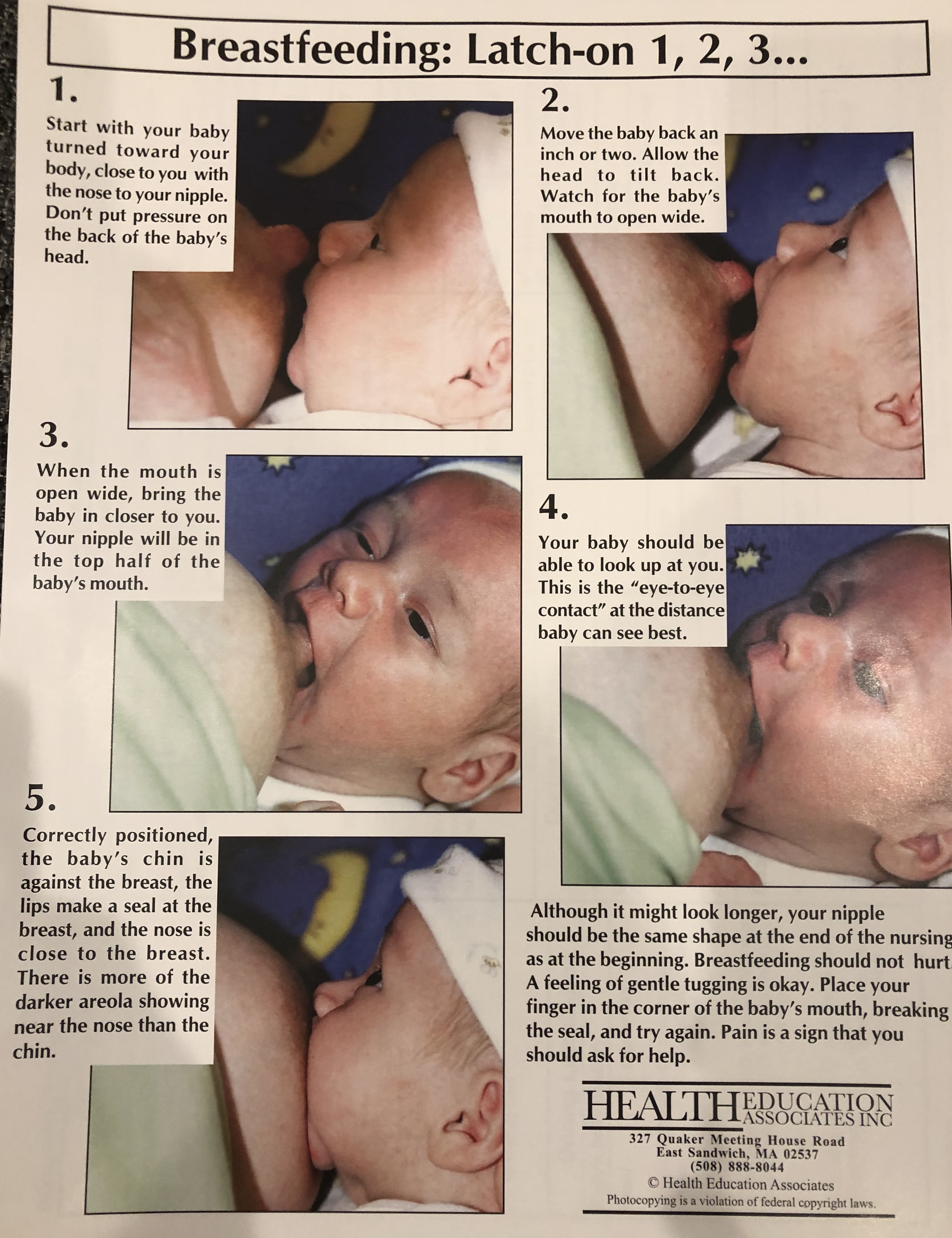
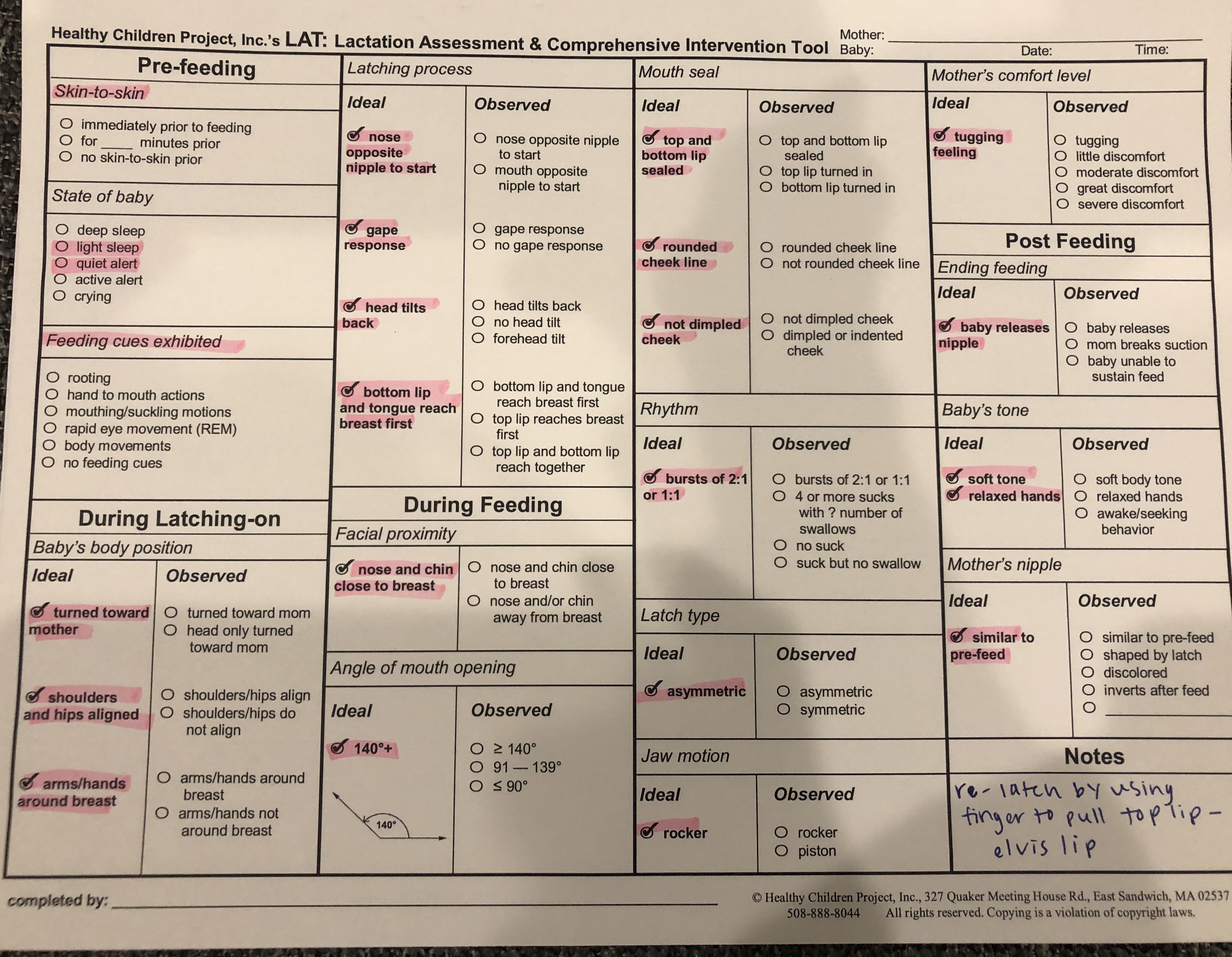
3. Get a Good Latch
- To start, line up belly to belly, nose to nipple, and tuck arms under belly if they get in the way (may squeeze a little breastmilk from nipple for baby to smell)
- Sandwich nipple and aim up at nose (thumb parallel with nose and nose exposed)
- Squeeze top of areola
- Move baby back an inch or two from nipple and let baby gape mouth wide (angle of mouth opening should be greater than 140 degrees)
- When baby’s mouth opens wide, push them in from the shoulders pressing forward and down so that chin and bottom lip hit the breast first
- Baby’s bottom lip and tongue should reach the breast first and nipple should fill the upper half of the mouth with the top of the areola exposed for an asymmetrical latch
- More of the lower part of the breast is drawn into baby’s mouth and nose and chin are close to the breast during feeding
- Top and bottom lip should form a seal around the breast (wet parts of lips will create a seal)
- Baby should have a rounded cheek line
- Baby’s hands should be around breast to stimulate oxytocin (milk let down)
- Two sucks to one swallow or one suck to one swallow ration during feeding
- Rocker jaw motion (moves whole breast tissue) versus up and down motion
- Remember, it’s not nipple feeding, it’s breast feeding
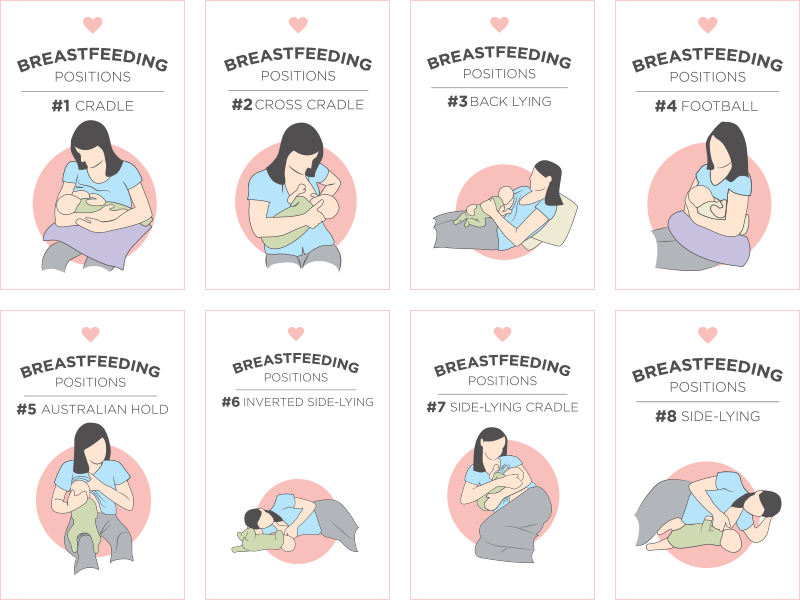
- Best positions for newborns: cross-cradle, football hold, laid back
- If baby tends to be too sleepy to feed, change their diaper, get them naked or play tug-o-war with finger in the baby’s mouth
If the latch is not correct, re-latch baby by hooking finger in baby’s mouth and around nipple to break the seal. May also pull up top lip (Elvis lip) to break the seal as well.
Baby is typically satisfied with feeding when they release nipple on their own, they have a soft, relaxed body tone and hands, and mother’s nipple loops similar to pre-feeding shape.
Click on images to print Latch resources.
4. Position Baby for Breastfeeding Success
Positioning Poem
“Tummy to Mummy, Nose to Nips
Flex Hips. To Open Lips”
Do not force your breast in your baby’s mouth or place hand behind baby’s head. The dark color of the areola and the amniotic fluid scent from the Montgomery glands will direct baby to the breast to feed. Here are some of the best positions for feeding that can also help your baby get a steady milk flow.
If you have an oversupply of milk, the back lying position may be helpful for baby to pace the feeding and work against gravity. Start lying back against a pillow and support elbow of feeding side with a pillow or prop. Babies head should be rested in the crease of your elbow and belly should be rested on your pelvis. Make sure baby’s nose is aligned with nipple and you place your fingers in a scissor shape along your nipple to flip into baby’s mouth making sure their is space under baby’s chin to swallow. If baby tends to feed fast, aim for 10 minutes on each breast to prevent engorgement. Side lying position also works well especially when Mom and baby are tired during the night.
5. If Problems Arise, Reset
Of course, there may be problems that arise in our life that can make breastfeeding difficult such as plugged ducts, mastitis, or low milk supply from travel or being out of routine.
Skin to skin is truly the best remedy for everything. It helps to soothe the baby, prevents fussiness, stimulates GI hormones, improves digestion and stimulates a healthy milk supply.Skin to skin neurologically centers the baby. It’s also a great activity for Dad to do for bonding and connection. Other great bonding opportunities for Dad include little pampering sessions (nail filing, hair brushing, and bath time.
Some woman re-establish exclusive breastfeeding by doing skin to skin with the baby in the bath tub. The bath water can mimic the birthing fluid to help baby re-learn the feeding process. Another tip for baby to relearn breastfeeding is to set a routine of bath, boob, and bed. This is especially great for fussiness.
6. The Right Amount To Feed Per Day
- 8-12 feedings/day, less than 140 minutes total
- 20-40 minute feedings (about 10-20 minutes each breast)
- Always offer baby each breast at each feeding to prevent engorgement (Sometimes newborns can get by on milk supply from one breast depending on how much you produce)
- Feeding should not exceed 45 minutes
- Women vary in amount of milk they make per day, but most women make at least 32 ounces of milk to supply their baby with the recommended daily needs
7. Feed At The Right Time
Babies cycle through 4 sleep/wake stages every 20-30 minutes and it’s important to feed the during specific cycles to ensure successful feedings.
- Deep Sleep. This is when the baby is out cold. Don’t attempt to feed during this time.
- Light Sleep State. This is the REM (rapid eye movement) stage and it is the best time to feed. Look for eye balls moving under eye lids and slowing bring baby to breast. REM sleep in babies is much lighter than REM sleep in adults. Sleeping baby’s cycle into REM sleep every half hour or so.
- Quiet Alert. This is when the baby is still and has fixed eye contact. This is also a good state to begin feeds.
- Active Alert. This is when the baby grows restless with hand to mouth activities, open eyes and rooting. This is a more difficult state for beginning feedings, but it can be done.
Crying is the worst time to put baby to the breast and typically means that you have missed babies earlier hunger cues. When baby cries, tongue moves the roof of the mouth and makes it very difficult for baby to latch onto the breast. Attempt skin to skin contact and wait 30 minutes until baby moves into a better sleep/wake stage for feeding. REM and quite alert states are the best stages for feeding. If you find your baby is too sleepy to feed, change their diaper, get them naked and try again.
8. Avoid Cracked Nipples & Nipple Pain
Avoid wiping nipples off after breastfeeding. There is a sebum oil that is produced from the small bumps around the areola called Montgomery glands that lubricate the nipples to prevent cracking while providing an antimicrobial property to prevent infection. These glands also secrete the scent of amniotic fluid, which helps baby know your breasts are where they can find food. This sebum oil provides an emollient affect that softens and relaxes the nipple while providing a soothing affect to the skin. If you have cracked nipples, simply express a little breastmilk and let it sit on the nipple until dry. Unrefined coconut oil can also be used to provide relief on nipples.
9. Feed When Baby Exhibits Hunger Cues
Rely on baby cues and feed during ideal sleep/wake stages. Babies also show more cues when they are close to their mother. Hunger cues include:
- Rooting (baby turning face towards stimulus and makes suckling motions)
- You can also stroke the baby’s cheek to stimulate natural rooting reflux of turning towards the breast
- Hand to mouth movements
- Smiling and eye contact
- If cues are missed or state is not optimal, re-introduce skin to skin.
10. Have Peace of Mind Knowing Baby Is Getting Enough Milk
- Baby stops losing weight by day 3 and begins to gain 1 ounce per day.
- By week 2, the baby should have regained to its birth weight.
- Baby should have a 1-ounce daily weight gain for the first month.
- Baby should have 4 soiled diapers by day four and each day thereafter.
- Several bowel movements each day from day 2 through the first 6 weeks.
- 3-5 urines and 3-4 stools per day by 3-5 days of age; 4-6 urines and 3-6 stools per day by 5-7 days of age.
- Baby has periods of quiet alert stage and seems content in between feedings.
10 Breastfeeding Myths
1. Breastfeeding Hurts
Although we have normalized breastfeeding as painful and hard, breastfeeding shouldn’t hurt. Nipple tenderness can be normal for the first few weeks but cracking, bleeding, bruising is a sign that baby isn’t latched on correctly. Also, when baby has an asymmetric latch it allows the tongue to rest on the bottom of the mouth and create a vacuum seal to allow milk transfer and prevent baby’s tongue or gums from rubbing on the nipple.
To ensure successful breastfeeding it is recommended to avoid nipple shields. As mentioned earlier, milk is made by nipple stimulation. A plastic nipple shield does not stimulate the nipple the same way the baby does through sucking or touching.
If you have clogged or plugged ducts, mastitis or other breast pain, consult a certified lactation consultant and continue to feed as much as possible. A hot shower or bath can also relieve pain and help milk let down and flow.
2. Pump and Dump
If there is alcohol in your blood stream, there is alcohol is breastmilk. Milk is not stored in the breast and is instead constantly flowing through the mammary glands and milk ducts. There is no way to control emptying out only the milk that contains the alcohol. If breastfeeding, it is recommended that you limit alcohol to less than 8 ounces of wine, 2 cans of beer, and 2 ounces of liquor in a two-three-hour time span. Less than 0.02 alcohol content is suggested to be safe for baby however, baby may not like the taste of the alcohol in the breastmilk which could make breastfeeding more difficult. The institute of medicine says that if alcohol is used, lactating woman should limit intake to no more than 0.5 g of alcohol per kg of body weight per day. Too much alcohol can also lower oxytocin levels and make it hard to move milk out of breasts eventually decreasing milk supply. If you are planning to drink alcohol, aim to nurse the baby before drinking and nurse again 2-3 hours after alcohol intake. In general, it’s said that if you are sober enough to drive, you are sober enough to breastfeed. Less than 2% of the alcohol consumed by the mother reaches her blood and milk. Alcohol peaks in Mom’s blood and milk approximately half an hour to one hour after drinking.
3. Foremilk & Hindmilk Contain Different Properties
In research studies, the milk at the beginning of a feed is called “foremilk” and the milk at the end of the feed is called “hindmilk.” Foremilk was said to contain more energy rich carbohydrates and the hindmilk was said to contain more satiety containing fat. For this reason it was said to completely empty each breast at feeding. As mentioned above, breastmilk is constantly flowing and does not have a storage capability in the breast. Foremilk and hindmilk can in fact have equal amounts of fat and other properties. The fat content actually varies throughout the day. When lactose and fluid volume are high, fat is low. Women tend to have thinner carb rich milk in the morning and thicker fat rich milk at night according to their circadian rhythms.
Also, faster milk removal from the breast increases fat content. Expressing your milk manually or using your hands when feeding or pumping to release milk ducts, does increase the fatty content of milk. (Fat tends to stick to the milk ducts, and using your hands can help release this into the milk).
With that being said, don’t worry about completely “emptying” the breast and use babies hunger cues when feeding. Baby will stop feeding when they are satisfied or ready to switch to the other breast. Some newborns may just stop sucking but stay latched on the breast. This is a good indicator they are done with feeding and you can use your finger to unlatch them from the breast.
If you do feel like you still have a lot of milk left in the breast after feeding, or your breasts are engorged, try pumping each breast immediately after a feeding. A small massager works well to release milk from engorged milk ducts. You can also bend forward and use your hand to rub the sides of your breasts to loosen up the breast tissue and help with milk flow. This can also help to mix up the milk. Personally, I’ve found it helpful to actually feed completely on one breast for a solid 20 minutes and only offer the second breast as “dessert” if baby needs a little extra something. This has allowed me to feel less engorged and ensure that the baby gets a good solid milk feeding. Less engorged breasts are also easier to feed from. By 6 months, I was offering both breasts at each feeding to make sure Brady was getting about 6 ounces (3 ounces from each breast). Typically, I would take a few minute break before switching to the next breast to burp him. He became very efficient at emptying each breast and unlatching naturally when finished.
4. Lack of Rest Lowers Milk Supply
Lack of rest and maternal exercise is not associated with decreased milk supply and the body will make enough milk regardless. When baby suckles on the breast and there is skin to skin contact with the mother, this activates the parasympathetic nervous system causing an increase in satiety hormones, gastrin and CCK allowing Mother to get into a deeper sleep even if it is just for 30 minutes. Stress does not directly lower milk supply however it may alter Mom’s behavior which can indirectly lower milk supply. Compared to formula feeding mothers, breastfeeding Mom’s tend to have more positive moods and less perceived stress due to the release of calming hormones like gastrin, CCK, and oxytocin. They also have less risk of having postpartum depression.
Also, breast size, diet, and fluid intake doesn’t affect milk supply contrary to popular belief. Of course, having a healthy diet and drinking enough fluids is recommended to keep Mom energized and happy while preventing bone loss and other nutrient deficiencies.
The biggest factors that affects milk supply is long spaces between feedings, long, slow feedings, excessive pressure on the breast (restrictive bras and clothing), and smoking.
5. Pumping Is The Best Way To Collect Milk
A baby is the best breast pump ever made and stimulates milk making and milk let down hormones in a way no pump can. When it comes to expressing milk, manual expression is actually the best way to collect milk due to nipple stimulation (prolactin) and skin to skin nipple contact (oxytocin) during the first few days after delivery. Manual expressed milk also contains higher fat content than milk pumped with an electric pump and may keep baby satisfied for longer. Ideally, it’s best to catch the milk in a cup and feed baby through cup feeding or small syringe versus a bottle to avoid nipple confusion early on. To manually express milk, start by placing your fingers 2-3 cm away from the nipple and squeezing breast tissue down towards the areola. Do this until stream stops and reposition hands to different areas around the breast. Milk ducts are around the entire areola so make sure to work through the entire breast.
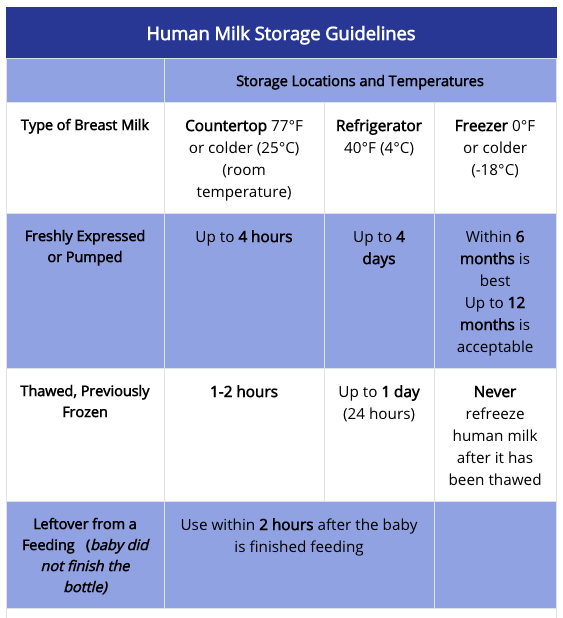
After the first few days, an electric breast pump may be helpful to relieve engorgement and reserve milk in a bottle for late night partner feeds. You may st0re expressed milk in a bottle or milk bag in the refrigerator for 3-5 days or store in a refrigerator freezer for up to 3 months or 6 months in a deep freezer. To prepare frozen milk, thaw in the refrigerator or warm in a plan of lukewarm water or under lukewarm running tap water. Thawed breastmilk should be used within 24 hours of being defrosted and should not be refrozen. If milk is room temperature, use within 4 hours. Discard leftover expressed breast milk or formula from feeding as it can contain bacteria from baby.
6. Baby Cries When Mom Leaves Because She Holds Them Too Much
Separation anxiety is due to object permanence and not from the Mom holding baby too much. (There is no such thing as cuddling your baby too much) Before going back to work, start playing hide and seek games and hide toys under blankets to let baby know object permanence is just temporary.
7. Fenugreek & Herbal Teas Can Stimulate Milk Production
Galactagogues are substances or herbal remedies believed to increase milk production. These include teas like chicory, orange spice, peppermint, raspberry, red bush, rose hips, and fenugreek. However, research has shown that there is no evidence of increased prolactin or milk production from consuming these herbs. However, Malunggay/Moringa has been shown to increase milk supply. Soy lecithin has also been shown to break up plugged ducts.
8. Baby Functions Best On A Set Schedule
Newborns cannot be expected to be on the same schedule as adults. They are just learning how to live in this new world outside of the womb and need time to figure things out on their own. However, a routine may be helpful in establishing feedings and a sleep cycle versus a set schedule. Routine has some regularity and provides stability while a schedule is set process with specific events and times that can be unrealistic for Mom and Baby to follow. The first 28 days are the most crucial for establishing a routine and getting the newborn acquainted with the world (and its parents).
During pregnancy I read a book that focused on feed/wake/sleep cycles and I found it to be so confusing and complicated. I felt like I had to write everything down and be so strict with this set schedule in order to have a happy, healthy baby. What I’ve learned is you have to just go with the flow, feed when the baby exhibits cues, and sleep when you can.
In the first week we found a routine that seemed to work well for keeping milk supply high and helping our son sleep through most of the night. Initially, newborns tend to have their days and nights mixed up but they will soon adjust. Try opening the shades during the day and dimming the lights at night. We also found that he slept better when he was swaddled or put in a sleep sack. For milk production and let down, it’s best to sleep with your newborn in your same room with a bassinet next to your bedside to listen for hunger cues. We found our son breastfed best when he was in a quiet alert state after a diaper change. Here’s a routine that worked for us although time does vary between 1-2 hours.
Newborn “Sleep Through The Night” Routine (Only Waking Up To Feed)
For the first 6-7 days, feed on demand all day/night every 2-3 hours. Around day 5 may you may have to pump to release extra milk and keep milk production high. I had an oversupply of milk and my breasts would be engorged if I didn’t pump in the morning and after the last nighttime feeding. During the days I would feed from one breast at a time or feed from one breast for 10-15 minutes and offer the second breast in case he needed some extra. During the night time feeds I always offer both breasts for 15 minutes each to sustain him for longer stretches. I estimated that each breast produces about 2.5 ounces of milk at one feeding based on how much I get during my pumping sessions and after weighing him before and after a feed at my lactation class. Ideally, your newborn will tell you when they are hungry and will be content when satisfied. The routine below is over a 24 hour period starting and ending with last nighttime feed with a total of 10-12 feedings per day (25 ounces total). This is roughly the schedule I followed for the first month.
- Breastfeed at 10:30pm (last night time feeding)
- Pump each breast for 15 minutes (5 ounces milk)*
- Reserve 2.5-3 ounces for middle of the night feed
- Bottle feed at 1:30am (from husband, try to avoid feeding a bottle yourself to avoid nipple confusion)
- Breastfeed at 4:00am
- Breastfeed at 7:000am
- Pump each breast for 15 minutes (5 ounces milk)
- Put in newborn boppy in bed and sleep in until 9:00am
- Breastfeed at 10:00am
- Breastfeed at 12:30pm
- Breastfeed at 3:30pm
- Breastfeed at 5:30pm
- Breastfeed at 8:00pm
- Breastfeed at 10:30pm
The partner bottle feed in the middle of the night was a life savor. Since I pumped right before bed I was able to go 6 hours without feeding and get a good chunk of rest. This also allowed my husband to bond with our baby and introduce him to a bottle while still putting milk from the breast first.
*Limit pumping after late night feeding if you have an oversupply of milk. Pumping will make your body produce even more milk. Starting by month two, my son was able to go 3-4 hour stretches of not feeding during the day and up to 6 hours at night, lowering the number of feeds to roughly 7-8 times/day.
By 6 months, Brady was eating about (5) 6 ounce bottles/day. He also became a much better nurser around 6 months which made life out and about so much easier. Sleep training also helped Brady to be a more efficient eater. We did the Little Z’s 6 month sleep training which was a 10 to 1 minute leave and check method. Brady was sleeping 11-12 hours by day 3!
9. Avoid Spicy Foods When Breastfeeding
Although food from the mother does not pass directly to the baby, the flavors do and babies actually appear to like stronger flavored breastmilk from foods containing garlic, herbs, and spice. Typically, the more diverse the Mother’s diet while breastfeeding, the less picky the child will be later on.
Cow’s milk whey is the only substance consistently shown to bother some babies, especially colicky babies. This is typically from cow’s milk versus cheese, yogurt, etc.
10. Avoid Caffeine When Breastfeeding
Caffeine consumption does not relate to the amount of caffeine in breastmilk and typically metabolizes in the blood stream before reaching the baby. Baby in utero usually absorbs more caffeine and other items that pass the blood brain barrier than with breastfeeding. Toxic exposure to infants occurs largely in utero and minimally through breast milk. As precaution, keep caffeine consumption to a minimum (below 300 mg/day) or avoid drinking if it affects your sleep and makes you irritable. One cup of coffee contains about 100 mg of caffeine and 2 ounces (2 shots) of espresso contains about 140 mg.
Nursing Strikes
Nursing strikes usually only last for a few days. Be patient and continue to offer the breast and nurse when able. Nursing strikes can happen for a number of reasons…
- A change in baby’s routine (Mom going back to work)
- Sign of illness (ear infection, fever, cold, stuffy nose)
- Teething
- Change in Mom’s fragrance, soap, etc.
- Warm temperatures outside (If baby is too hot this can make nursing very uncomfortable)
- Slow let down (Baby can be impatient especially if feeding from bottle at daycare)
- Sometimes when you switch to a bigger nipple size on the bottle, this can lead to nursing problems.
- You can express a little milk before you nurse to keep Baby engaged
- Sometimes for no good reason–Baby is just being stubborn
I experienced a nursing strike a few different times by the time Brad was 6 months old. The first happened out of no where and I couldn’t figure it out. This nursing strike also came with a period of fussiness and sleep challenges. Luckily, Brad’s 3 month doctor’s appointment was right around this time and we realized he had an ear infection which made all of his challenges make sense. Once we started taking his antibiotics, the pain subsided and he returned to nursing.
The second nursing strike happened for no good reason right around the time Brady started daycare. All of a sudden Brady wasn’t interested in nursing and kept pushing me away. He would take a bottle no problem and wasn’t experiencing any signs of illness. During the night I would nurse him while he was sleepy and the next day he seemed to forget about his nursing strike.
The third nursing strike happened when we went on family vacation. He refused to nurse and would get very upset when I put him in any nursing position. He was also going through a growth spurt at this time and I could barely keep up with his supply and demand through pumping and feeding him bottles. He was taking about a 6 ounce bottles every three hours even through the night. I think the nursing strike was due to being in a new location and also because it was extremely hot in the vacation home we were staying in. After 2 days and 2 nights of having to pump on demand and being up at all hours of the night I knew I had to figure something out. One night at 2:00am I started to pump while Brady was in his bouncer seat looking up at me. After expressing a few ounces into a bottle, I brought him to my nipple and he surprisingly latched on no problem. After that I began to express some milk on my nipples before bringing him to latch so he could smell the milk and know what was coming. After that we had no latching problems at all and he seemed to forget all about his nursing strike.
Around 6 months when we began sleep training Brady became a very efficient eater and seemed to love nursing–especially in the mornings.
Nursing Strike Remedies
- Change nursing positions
- Nurse in motion
- Skin to skin
- Express milk onto nipple before brining baby to latch
- Nurse after pumping session (Nipples are already stretched and milk will flow faster because of let down)
- Nurse when baby is sleepy or during the night in the dark
- If after a few days, baby still refuses to nurse, visit your pediatrician to rule out possible ear infections
- If baby only nurses from one breast, see your doctor to rule out possible breast issues
Clogged Ducts/Nipple Blisters
In the initial breastfeeding days when your milk comes in, your breasts may feel extremely full and engorged. If you aren’t emptying them adequately, you may get clogged ducts where areas on the breast feel hard and sore. The best way to relive clogged ducts is with a warm compress, hot shower, or soaking belly down in a bath to let gravity release the clog. It’s also helpful to feed or pump while massaging the clogged spots.
When Brady was 10 months I went on a week long trip to Europe with my husband where I pumped 3 times a day for a total of 22 times. I was emptying my breasts but not as effectively as if I was nursing and my circadian rhythm and milk production got all out of whack because of the time change. A few days after I got home and started nursing and pumping at my normal times, I started to get some major clogged ducts. My breasts were so lumpy and sore to the touch I was in constant pain. It took a good week of nursing to release these clogs and get back to normal. I also took many hot epsom salt baths while hand expressing to break up the clogs.
I also may have had a nipple blister from pumping so much. This usually happens when skin forms over the nipple pore and prevent milk from flowing effectively and can be very painful. The nipple is extremely sore and you may feel a throbbing like sensation when the baby feeds. The best remedy for a nipple blister is to soak the nipple in epsom salt water. I actually filled up a shot glass with epsom salt and placed it over my nipple before and after a feed. Eventually the skin that formed over my nipple peeled away and I cleaned the area just by squeezing breast milk from my nipple and continuing to soak in warm epsom salt water.
When all else fails just nurse, nurse, nurse. Your baby will be the most effective at releasing clogged ducts and healing a nipple blister.
Pumping & Going Back to Work
It’s important to wait until milk supply is established before pumping. Bringing your baby to breast is the number one way to increase milk supply and let down. Pumps do not stimulate the same hormones as human contact which can make pumping unsuccessful in the beginning. Once I established breastfeeding, I started pumping in the morning after the first feed to relieve engorgement and increase milk supply. Keep in mind the more you empty your breasts, the more milk your body will make.
Ideally, it’s best to start pumping at least 3 weeks before going back to work to establish a routine and start to collect a stash of breastmilk for when you’re away. Here are some tips for keeping milk supply up while returning to work.
- Breastfeed before leaving for work and when returning from work to increase milk producing hormones, prolactin and oxytocin
- Be available to nurse baby as much as needed after work and on weekends (offer extra skin to skin contact)
- Pump both breasts at the same time
- Try to go back to work on Thursday versus a Monday to give body time to adjust away from baby
- Baby needs about 1 ounce every hour baby is away from Mom (Breast makes about 1.25 ounces/hour)
- Offer 3- 5 ounces per feeding (average 4 ounces)
- From 1-6 months of age, babies need anywhere from 19- 30 ounces/day
- Plan to pump about 15 ounces during a work day, 30 ounces for 24 hours/overnight
- This accounts for spillage, etc
- By 5 months, my son was taking (3) 6-7 ounce bottles at daycare which meant I needed to supply about 20 ounces while away from him
- Each breast makes about 1.25 ounces per hour (baby leaves 1/3 behind of what is available; therefore breasts are never completely empty)
- Appropriately sized flange is important for sufficient milk release (make sure pump flange provides space around the nipple and do not rub around the nipple causing irritation)
- Pump after first morning feed when milk supply is the highest (Prolactin is highest between 12:00-4:00am
- Pump with baby close to you to release more oxytocin and help with milk let down (look at photos/slideshow of baby if away)
- Don’t go longer than 4 hours during the day without feeding/pumping (releasing milk with keep supply high)
- Pump 2-3 times per day
- Personally, I was able to pump twice a day at 9:00am and 3:00pm because of my high milk supply
- Each pumping session I was able to get about 10 ounces (5 on each breast)
- May pump before bedtime ounce baby sleeps through the night (or longer than 6 hours) to prevent engorgement/clogged ducts/mastitis
- Power pumping can help to increase milk volume. Pump for 5 minutes, pause, pump for 5 minutes, pause and pump for 5 minutes
- Make sure you handle pump with proper CDC cleaning guidelines
- You may keep used pump parts in ziploc bag in the fridge to reuse within 24 hours, or use breast pump cleansing wipes when traveling
- When traveling, use Haakaa silicone suction pump for easy and noise free milk release or hands free pump such as the Willow or Freemie. You may also get a battery pack for electric pump.
- There is no need to change nipple size on bottle. A slower nipple flow can mimic the breast unless you have an extremely fast let down.
- If nursing strike happens where baby refuses the breast, try, try, and try again but don’t force it or get upset. Nurse when baby is sleepy or in motion, vary positions, and continue to do skin to skin. Sometimes if a baby is sick or has an ear infection they may not have the strength to breastfeed and a bottle can be easier. Staying positive is key.
- Use Packit cooler with built in ice pack to store ad travel with milk. Airport security allows breastmilk, breast pumps, ice packs, and dry ice to pass through simple screening tests.
- If weaning, take it slow by dropping one feed per week. Replace feed with frozen breastmilk. Feeding per day may naturally reduce if feeding baby solids.
- Use Lilypadz for leaking and seamless coverage as breast pads can be lumpy and wet.
Learn more at Womenshealth.gov
Breastmilk Storing Guidelines
- If baby doesn’t finish breastmilk bottle, keep in the refrigerator for 3-4 hours and give at next feed. If you have any leftover milk when the baby is finished feeding, it may also be kept at room temperature for 2 hours. After this time you must discard any unused milk and may not mix it with other breastmilk.
- If breastmilk has already been re-heated, you may keep it at room temperature for 4 hours. If it is not used, then it must be discarded and can not be reheated again.
- Once breastmilk is completely thawed, it must be used within 24 hours. (Keep in mind this is not from the time you pull the milk from the freezer, it is the time from when the milk is completely thawed. Example: you can pull frozen milk on Monday to store in the refrigerator to use Tuesday-Thursday. (Thaw frozen milk in the refrigerator or in a bowl of warm water).
- You may store frozen milk back in the freezer if it becomes slightly thawed.
- Once frozen milk is thawed and warmed, it can be kept at room temperature for 2 hours.
- Rule of 6
- Expressed breastmilk can be at room temperature for 6 hours. If you plan to use this after the 6 hours window, store in the refrigerator as soon as it’s expressed.
- Expressed breast milk can last for 6 days in the refrigerator. (Freeze by day 4-5)
- Expressed breast milk can last for 6 months in the freezer (12 months in deep freezer)
- Pumped milk can be mixed together during a 24 hour period.
- Only mix the same temperature milks. Do not mix chilled breast milk with freshly expressed milk as it can change the composition and denature nutrients.
- Store breastmilk bags flat or in storage organizer to save space.
It’s important to properly wash pump parts with soap and water or even Babyganics foaming dish and bottle soap after each use. I also like to run my pump after a pumping session to get rid of any condensation in the tubing. If using pump parts within 24 hours, you may store them in a ziploc bag in the refrigerator until the next use.
Formula 101
Do you know it costs only $0.25 to make a container of formula but costs you around $30.00-$50.00 per container? There are many lobbyist companies backing formula companies for profit since they know this is where Mom’s look to for adequate nutrition for baby when breastfeeding may not be an option. When it comes to formula marketing campaigns are one of the biggest reasons that formula is so expensive. It costs on average about $2,000/year to formula feed?
Did you know that formula companies only have to list the top 20 ingredients in their formula and can avoid lead, cadmium (carcinogenic metal), and arsenic disclosure? Keep in mind that soy formula has 6x more cadmium than cow’s milk formula. Compared with breastfed babies, those fed formula can be exposed to up to 12x the amount of cadmium and powdered formula is particularly susceptible to contamination.Formula also does not provide antibodies for the baby’s microbiome and can lead to poor gut health. Even just one bottle of formula can impact a baby’s gut long-term.Bottom line is that formula is not as nutritious as breast milk and we simply can’t always trust what we see on the label or on marketing campaigns.
The Hierarchy of Infant Feeding Choices
- Baby at Mother’s Breast
- Mother’s Own Expressed Milk
- Milk from Human Milk Banking Association of North America (HMBANA) or licensed milk bank
- Cow’s Milk Formula
- Soy Formula
Non-Species Specific Milk
We are the only species in the world that consumes another species milk such as cow’s milk. Human milk is one of the highest in lactose of all mammalian milks, high in water, low in protein and fat and is considered a very dilute mammal milk. Human milk is the ideal fuel for brain growth and developing grey matter. As humans, we do not have the right enzymes to break down cow’s milk which ultimately leads to digestion related disorders, asthma, and auto-immune issues.
The bioavailability of nutrients in human milk are higher than that of other foods and supplements. Formula typically is fortified with iron which is not as bioavailable as breast milk and can cause constipation. Babies are actually born with enough iron and vitamin D stores for 6 months after birth so there is no need to supplement if exclusively breastfeeding. With vitamin D however, many Mothers are deficient in vitamin D during pregnancy and while breastfeeding, which can affect the baby’s stores. While vitamin D and DHA (a brain-boosting omega 3 fat) are important for newborns, these nutrients can pass through from the mother to the baby when breastfeeding. For this reason, it is extremely important to supplement with a good quality cod liver oil during pregnancy and post-partum to ensure healthy nutrition for Mom and baby. Cod liver oil contains the perfect balance of vitamin D and omega 3s. I also recommend add baby probiotics to a bottle or in the baby’s mouth using a dropper if they tend to have bad gas.